COVID-19 Second Wave Risk: Best and Worst States [Healthcare & 2026 Readiness Ranked]
With experts predicting a serious COVID-19 second wave risk, New Mexico ranks as the least prepared state. New Mexico faces many challenges caring for its residents during COVID-19, with only 1.8 hospital beds per 1,000 people and 17.5 percent of its population over 65. The state best prepared for the second wave of COVID-19 is Minnesota, which has 2.5 hospital beds per 1,000 people and 303 active physicians per 100,000 people.
Read moreFree Life Insurance Comparison
Compare Quotes From Top Companies and Save
Secured with SHA-256 Encryption
Jeff Root
Licensed Insurance Agent
Jeff is a well-known speaker and expert in life insurance and financial planning. He has spoken at top insurance conferences around the U.S., including the InsuranceNewsNet Super Conference, the 8% Nation Insurance Wealth Conference, and the Digital Life Insurance Agent Mastermind. He has been featured and quoted in Nerdwallet, Bloomberg, Forbes, U.S. News & Money, USA Today, and other leading...
Licensed Insurance Agent
UPDATED: Dec 9, 2023
It’s all about you. We want to help you make the right coverage choices.
Advertiser Disclosure: We strive to help you make confident insurance decisions. Comparison shopping should be easy. We are not affiliated with any one insurance provider and cannot guarantee quotes from any single provider. Our insurance industry partnerships don’t influence our content. Our opinions are our own. To compare quotes from many different companies please enter your ZIP code on this page to use the free quote tool. The more quotes you compare, the more chances to save.
Editorial Guidelines: We are a free online resource for anyone interested in learning more about life insurance. Our goal is to be an objective, third-party resource for everything life insurance related. We update our site regularly, and all content is reviewed by life insurance experts.
UPDATED: Dec 9, 2023
It’s all about you. We want to help you make the right coverage choices.
Advertiser Disclosure: We strive to help you make confident insurance decisions. Comparison shopping should be easy. We are not affiliated with any one insurance provider and cannot guarantee quotes from any single provider. Our insurance industry partnerships don’t influence our content. Our opinions are our own. To compare quotes from many different companies please enter your ZIP code on this page to use the free quote tool. The more quotes you compare, the more chances to save.
On This Page
The Truth in a Nutshell
- Researchers say that the second wave of COVID-19 could be just as bad as the first
- States with an older and more immunocompromised population are especially at risk
- States with better medical infrastructures are better prepared to face a pandemic
- We rank Minnesota as most-ready and New Mexico as least-ready for COVID-19’s second wave
Now that the first wave of the coronavirus is slowing, states are beginning to reopen all sorts of businesses and their economies in general.
But according to the American Medical Association, “Summer may slow the spread of the coronavirus a bit, but it will be back by fall with a second wave that looks a lot like the first wave.”
In fact, many researchers have said this second wave of COVID-19 infections could be even worse than the first. In this article we cover the 10-most prepared and 10-least prepared states for a COVID-19 second wave risk.
We’re all learning how to cope with this new pandemic, from protecting our homes and cars against COVID-19 to learning how to teach our children online and at home as schools close. But the threat of a second wave of the coronavirus outbreak led us to ask: What states are best-prepared to face the second wave of the coronavirus?
We’ll rank the 10 most prepared states and the 10 least prepared states. We’ve done the research on how each state’s medical infrastructure and resident health statistics make them prepared or more at risk to face a pandemic.
It’ll be a bit like looking at the coronavirus by state, the coronavirus curve by state, coronavirus trends by state, and the top states with coronavirus.
The coronavirus pandemic has done more than test each state’s healthcare system. It also has had an impact on industries across the US economy, including the insurance industry. If you’re looking for insurance, plug your information into our FREE quote comparison tool to receive the best quotes for you and your area before the COVID-19 second wave risk.
Of course, we understand that insurance can be confusing with all the technical terminology, different parts of plans, and the number of options you have. If you are looking for more information in general about insurance or need something clarified, check out our insurance topics page that contains answers to dozens of insurance questions.
Predicting the impact of coronavirus is an impossible task. But we can dive into how states are preparing (or not preparing) for their next outbreak season and rank the states most and least prepared for the risks associated with COVID-19’s second wave.
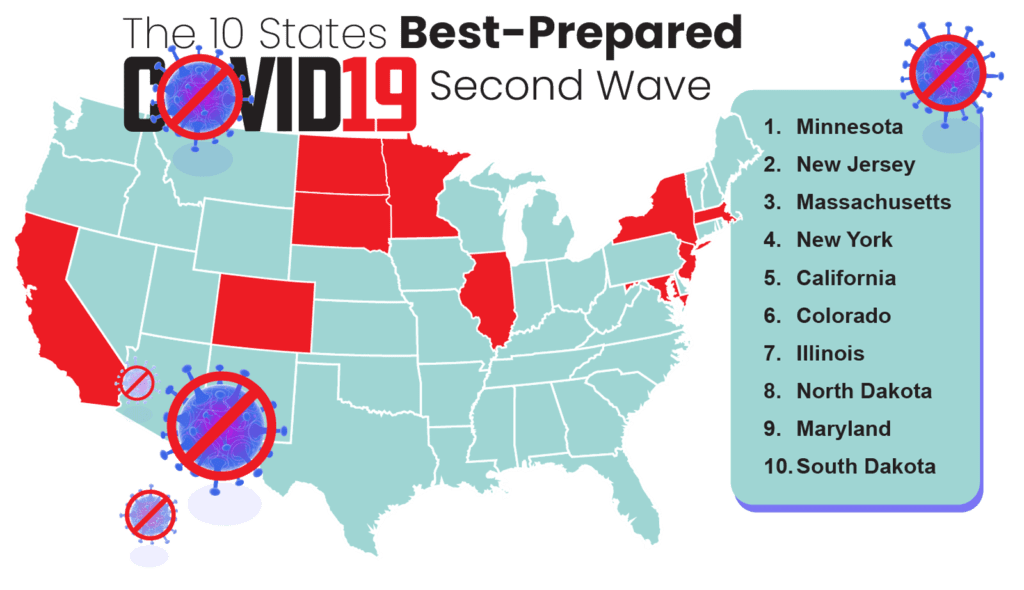
10 States BEST Prepared for the 2nd Wave of the Coronavirus
When it comes to pandemic preparedness, not all states are equal in their guard against coronavirus. A state’s preparedness is based upon not only its medical infrastructure—such as the number of hospital beds per capita—but also the overall age and health of its citizens. And beyond these factors, individuals must enact responsible behaviors to prevent COVID-19.
Read More: Coronavirus & Responsible Behaviors by State
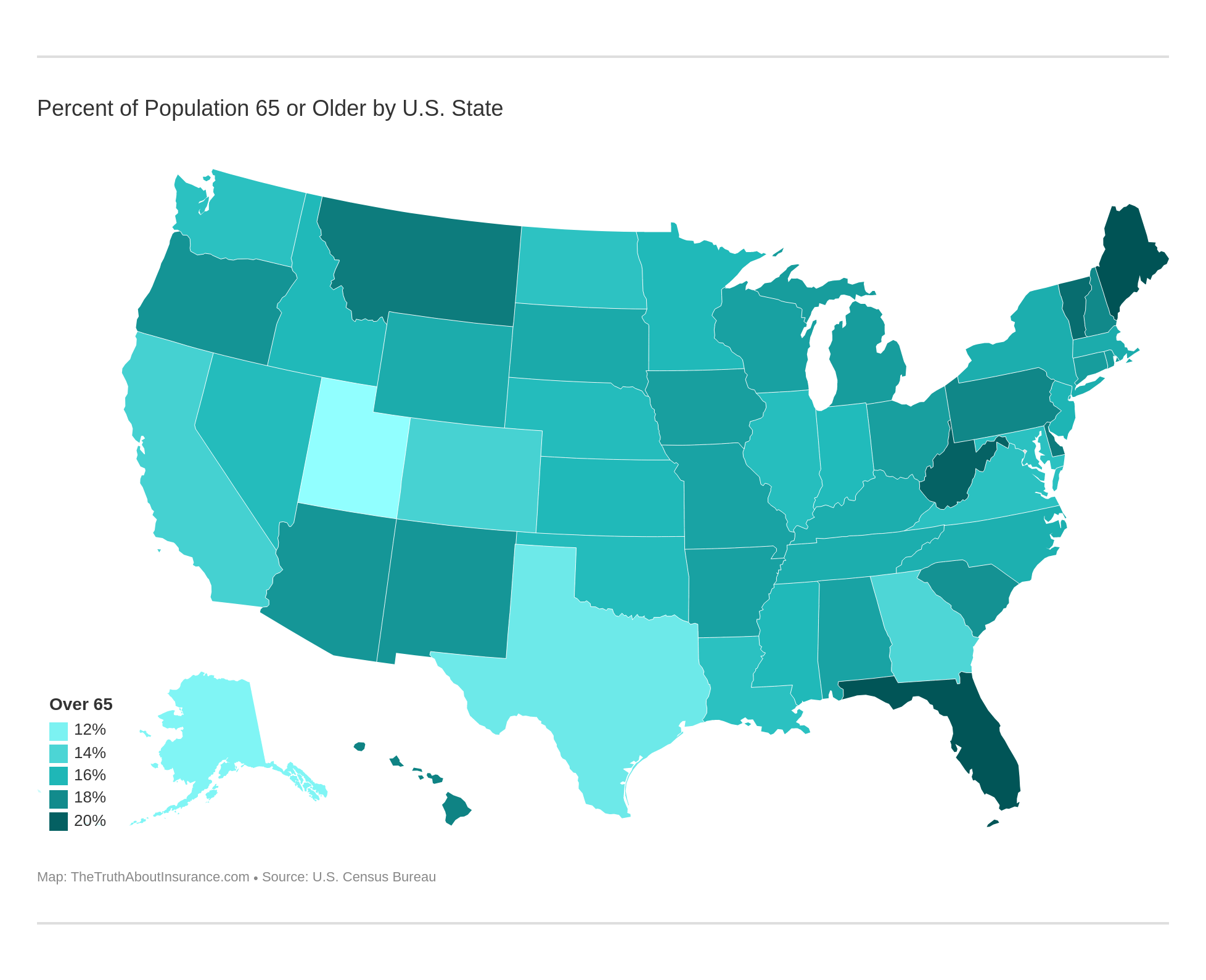
As you can see in the interactive map below, states do not have an even age distribution across the United States. This is important to know because seniors are especially at risk for contracting and suffering severe cases of COVID-19.
It’s true: Certain age groups, particularly those over the age of 65, and folks with certain pre-existing health conditions are at a higher risk of becoming infected with the coronavirus. The Centers for Disease Control and Prevention (CDC) explains that those most at-risk for severe illness from COVID-19 include people 65 years and older as well as those who:
- live in a nursing home or long-term care facility
- have chronic lung disease or moderate to severe asthma
- have serious heart conditions
- are immunocompromised
- face severe obesity
- have diabetes
- suffer from chronic kidney disease undergoing dialysis
- have liver disease
To rank which states are best- and least-prepared to face a second wave of the coronavirus, we looked at six primary factors. These factors include a state’s share of residents over the age of 65 and its share of residents facing certain health conditions such as asthma and obesity. We also consider medical infrastructure statistics such as the number of hospital beds and active physicians per capita, as well as the share of residents who don’t have health insurance.
In the table below, we share the 10 states best prepared to face another round of coronavirus infections, ranked beginning with the most prepared.
10 States Best Prepared for COVID-19’s Second Wave
| State | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents | Rank |
|---|---|---|---|---|---|---|---|
| Minnesota | 15.9% | 8.3% | 30.1% | 2.5 | 302.7 | 5.1% | 1 |
| New Jersey | 16.1% | 8.4% | 25.7% | 2.4 | 306.5 | 9.0% | 2 |
| Massachusetts | 16.5% | 10.2% | 25.7% | 2.3 | 449.5 | 3.3% | 3 |
| New York | 16.4% | 10.1% | 27.6% | 2.7 | 375.1 | 6.6% | 4 |
| California | 14.3% | 8.5% | 25.8% | 1.8 | 279.6 | 8.2% | 5 |
| Colorado | 14.2% | 9.1% | 23.0% | 1.9 | 285.7 | 8.7% | 6 |
| Illinois | 15.6% | 8.7% | 31.8% | 2.5 | 284.4 | 7.9% | 7 |
| North Dakota | 15.3% | 8.2% | 35.1% | 4.3 | 237.6 | 8.6% | 8 |
| Maryland | 15.4% | 9.3% | 30.9% | 1.9 | 386.0 | 7.0% | 9 |
| South Dakota | 16.6% | 2.9% | 30.1% | 4.8 | 240.4 | 10.8% | 10 |
Many of these states are probably not surprising. States like Minnesota and Massachusetts are known for their medical treatment and research centers. But some states, like North Dakota and South Dakota, may be more surprising to see on our list of states best prepared to face another round of the coronavirus. Let’s take a closer look.
Compare Quotes From Top Companies and Save Secured with SHA-256 Encryption
#10 – Prepared: South Dakota
Starting off our countdown of the 10 states best prepared for another round of coronavirus infections is South Dakota.
This sparsely populated state in the upper Midwest may be a surprising inclusion here, but fewer South Dakotans struggle with asthma than residents of any other state. That’s a key factor when thinking about a respiratory virus like COVID-19. Additionally, with 4.8 hospital beds per 1,000 residents, the state has more hospital beds per capita than any other state.
South Dakota Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 884,659 | 16.6% | 2.9% | 30.1% | 4.8 | 240.4 | 10.8% |
South Dakota does have several key industries that face high rates of coronavirus transmission. As you can see in the video from CBS News below, for instance, workers in the meatpacking industry are especially at risk when it comes to COVID-19.
With hundreds of workers infected in a single location, then going out in the world and exposing their families and neighbors, we can see how every state, despite how prepared they are, is at risk for a pandemic as contagious as COVID-19.
When it comes to public safety, we’ve ranked South Dakota highly before. In our most dangerous cities to drive ranking that found Washington DC is the most dangerous place to drive, we covered the safest cities to drive in as well. The top one was Sioux Falls, South Dakota.
#9 – Prepared: Maryland
Home to the Johns Hopkins University Medical School, U.S. News & World Report’s second-best medical school in the nation, the state of Maryland also has the second-most number of active physicians per capita of any state.
Maryland Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 6.046 million | 15.4% | 9.3% | 30.9% | 1.9 | 386 | 7% |
With fairly high rates of asthma, not surprising given Maryland’s industrial core and location along the busy Mid-Atlantic corridor, the state faces some difficulty when it comes to respiratory problems in general—problems that can become easily complicated or even deadly when combined with a coronavirus outbreak.
Geico, one of the largest insurance providers in the United States, is headquartered in Chevy Chase, which means many Marylanders work in the insurance industry. To this end, check out this guide that we’ve created on insurance industry expectations, so you know what to expect when working in the insurance industry.
#8 – Prepared: North Dakota
Like its neighbor to the south, North Dakota has a lot of hospital beds—4.3 for every 1,000 residents—ready to treat COVID-19 infections when a second wave hits. The Peace Garden State also has a relatively low share of uninsured residents.
North Dakota Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 762,062 | 15.3% | 8.2% | 35.1% | 4.3 | 237.6 | 8.6% |
In the video below, North Dakota Governor Doug Burgum is moved to tears over the misinformation regarding the coronavirus and the resistance by some to simply wear masks as a preventative measure.
Do face masks help reduce the transmission of the coronavirus? Absolutely. When asked this question, the Mayo Clinic answered emphatically:
“Yes, face masks combined with other preventive measures, such as frequent hand-washing and social distancing, help slow the spread of the virus.”
Even though North Dakota is well-prepared to face the second wave of COVID-19, other public safety concerns plague the state. Currently, North Dakota is the second-worst state for drunk driving in the Midwest as seen in our 30 million drunk drivers on US roadways article.
#7 – Prepared: Illinois
Illinois’ largest city, Chicago, has been a hotspot in the first wave of the coronavirus pandemic. But with a high number of hospital beds per capita and a relatively low number of uninsured residents, we believe the state is well-prepared to face the second wave of COVID-19.
Illinois Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 12.67 million | 15.6% | 8.7% | 31.8% | 2.5 | 284.4 | 7.9% |
The State of Illinois updates its response page daily. The page provides not only a county-level interactive map of COVID-19 cases but also resources for getting tested and treated.
Interesting fact: Illinois is also home to State Farm, the largest car insurance provider in the United States. With headquarters in Bloomington, Illinois, State Farm holds more than 17 percent of all car insurance policies in the nation.
#6 – Prepared: Colorado
The state of Colorado has a relatively young population that has the lowest obesity rates of any state in the nation, both factors that help prepare it to face another round of COVID-19 infections.
Colorado Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 5.759 million | 14.2% | 9.1% | 23% | 1.9 | 285.7 | 8.7% |
Though Colorado’s number of hospital beds per capita is fairly low, it does have an average number of active physicians and a low rate of uninsured residents. Cities across the Mile High State are taking the coronavirus pandemic seriously. In the video below, you can catch a glimpse of how the Colorado city of Telluride contained the COVID-19 virus and protected its residents.
Of course, economic and health measures are sometimes at odds in fighting this virus, especially in a tourist-focused state like beautiful Colorado. But as we face another round of this pandemic, it’s essential that all localities take active measures to protect residents and visitors alike.
#5 – Prepared: California
California, and especially Los Angeles County, was one of the hardest-hit places in the first round of the COVID-19 crisis. Luckily, the most populous state in the nation has a strong medical infrastructure, which helps prepare it to face another round of coronavirus infections.
California Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 39.51 million | 14.3% | 8.5% | 25.8% | 1.8 | 279.6 | 8.2% |
In the first round of the coronavirus pandemic, California took strong measures to protect its residents. Though these measures are starting to let up, we expect stay-at-home orders and other measures to come back strong when the second wave of COVID-19 hits.
With so many Californians transitioning to working remotely, it’s important to consider increased risk factors that can affect personal safety and public health. For instance, California is already one of the top ten states for dog bite insurance claims in the United States. With more residents spending time at home or at dog parks with their pets, the number of claims could increase even more.
#4 – Prepared: New York
In the fourth spot of our ranking of the states best prepared to face a second wave of the coronavirus is the Empire State. New York has a lot of active doctors and a low percentage of uninsured residents, both signs that point to pandemic preparedness.
New York Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 19.45 million | 16.4% | 10.1% | 27.6% | 2.7 | 375.1 | 6.6% |
Nearly half of New York residents live in and around New York City. New York City was the hardest-hit city in the first round of coronavirus infections, and as you can see in the video below, the pandemic has had a tragic effect on the City that Doesn’t Sleep.
Luckily, the State of New York and New York City have worked together to better prepare for a second wave of the COVID-19 virus. That’s good news for not only New Yorkers, but also the nation, given New York City’s status as a center for banking, trade, and other key industries.
#3 – Prepared: Massachusetts
With more doctors than any other state in the nation and an extremely low share of uninsured residents, the Commonwealth of Massachusetts is well-prepared to face another wave of COVID-19 head-on.
Massachusetts Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 6.893 million | 16.5% | 10.2% | 25.7% | 2.3 | 449.5 | 3.3% |
Massachusetts is also home to some of the world’s finest medical institutions, such as the top-ranked Harvard Medical School. Harvard Medical School has been at the forefront of public information surrounding the coronavirus. The video below comes from their series “Coping with Coronavirus,” and focuses on emotional health during this difficult time.
As we all prepare for the second wave of COVID-19, it’s important to focus on mental health, both individually and collectively. Resources like this YouTube series from Harvard Medical School are available to folks around the world, not just residents of the Bay State.
#2 – Prepared: New Jersey
Across the board, New Jersey shows lots of solid signs of pandemic preparedness, from a relatively young population to a mostly-insured citizenry. Additionally, the state has a high number of active physicians compared to most other states.
New Jersey Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 8.882 million | 16.1% | 8.4% | 25.7% | 2.4 | 306.5 | 9% |
New Jersey is also densely populated. Though a dense population poses a higher risk for quicker virus spread, it also means easier access to testing and treatment centers. States with larger urban-rural divides struggle to build easy access to testing and treatment centers.
Though we rank New Jersey as one of the states best prepared to face another round of coronavirus infections, it’s not necessarily one of the safest states for drivers. In fact, we recently found drivers in Newark, New Jersey to exhibit some of the highest accident risks of any drivers across the country.
#1 – Best Prepared State: Minnesota
With a great medical infrastructure and a relatively young population, Minnesota takes the top spot in our ranking of the states best prepared to face a second wave of the coronavirus.
Minnesota Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 5.64 million | 15.9% | 8.3% | 30.1% | 2.5 | 302.7 | 5.1% |
Minnesota is home to the Mayo Clinic, one of the top-ranked and most-trusted medical research centers in the world. As the coronavirus has wreaked havoc on the United States, the Mayo Clinic has stepped up to provide accessible and essential health information such as the Q&A video below.
As the second wave of COVID-19 infections looms, it’s important to turn to resources like the Mayo Clinic or CDC for reliable information that could save your life and protect your loved ones from this dangerous virus.
As we face this second coronavirus season, it’s important to make sure you have the right health insurance for you and your family. Though the open enrollment period to switch plans is typically between November 1 and December 15 of each year, the COVID-19 crisis may be deemed a qualifying event in many states. A qualifying event allows people to switch providers outside the usual period.
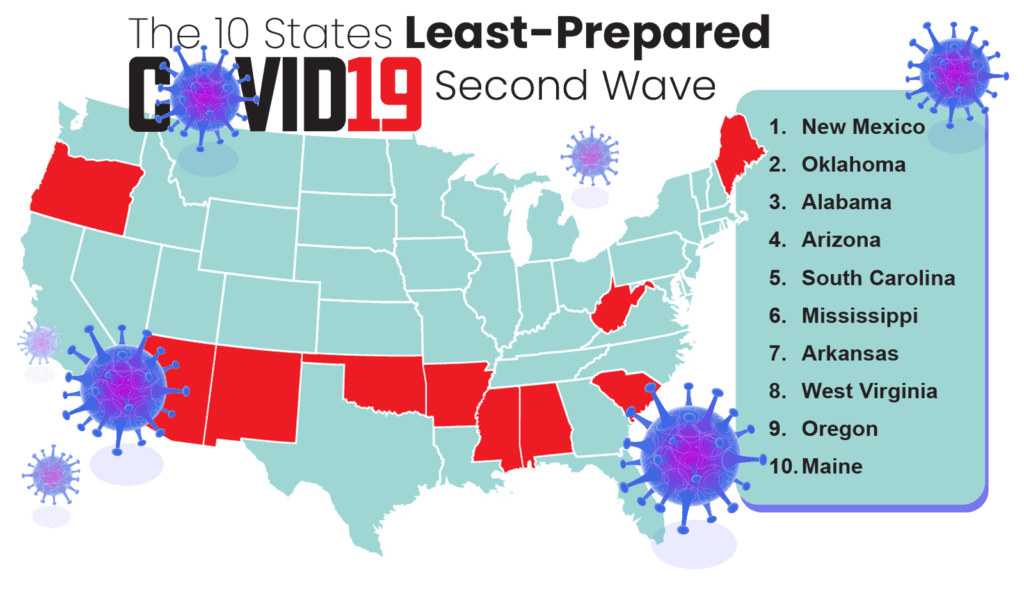
10 States LEAST Prepared for the 2nd Wave of the Coronavirus
As we stated above, not all states are equally prepared to face a public health crisis such as the second wave of COVID-19. So what states, you might be wondering, are least prepared?
As you can see, the states least-prepared to face a second wave of the coronavirus pandemic are mostly located across the American South and Sun Belt. Sadly, many of these states have high poverty and uninsured rates.
In the table below, we share information about the 10 states least-prepared to face another round of coronavirus infections.
10 States Least-Prepared for COVID-19’s Second Wave
| State | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents | Rank |
|---|---|---|---|---|---|---|---|
| Maine | 20.6% | 12.3% | 30.4% | 2.5 | 330.2 | 10.2% | 10 |
| Oregon | 17.6% | 11.6% | 29.9% | 1.6 | 303.4 | 8.2% | 9 |
| West Virginia | 19.9% | 12.3% | 39.5% | 3.8 | 263.4 | 7.5% | 8 |
| Arkansas | 17.0% | 9.8% | 37.1% | 3.2 | 207.6 | 9.3% | 7 |
| Mississippi | 15.9% | 9.7% | 39.5% | 4 | 191.3 | 14.5% | 6 |
| South Carolina | 17.7% | 9.1% | 34.3% | 2.4 | 229.5 | 13.1% | 5 |
| Arizona | 17.5% | 10.0% | 29.5% | 1.9 | 242.0 | 12.1% | 4 |
| Alabama | 16.9% | 10.5% | 36.2% | 3.1 | 217.1 | 11.0% | 3 |
| Oklahoma | 15.7% | 10.3% | 34.8% | 2.8 | 206.7 | 16.5% | 2 |
| New Mexico | 17.5% | 9.9% | 32.3% | 1.8 | 244.8 | 11.0% | 1 |
The biggest thing these states have in common not evident in this table? They all have a large urban-rural divide that makes strong medical infrastructures especially difficult to build. Let’s take a closer look at these 10 states.
#10 – Unprepared: Maine
One of two Northern states on this list, Maine has a largely rural population. Maine also has the largest share of residents over the age of 65 of any state across America. As most people know, this age group is at the highest risk of not being able to survive COVID-19 if they catch it.
Maine Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 1.344 million | 20.6% | 12.36% | 30.4% | 2.5 | 330.2 | 10.2% |
When a state has a large rural population, it tends to struggle to build medical infrastructures to serve its widely-spread population adequately. In the video below from MSNBC’s Rachel Maddow, the slow but dangerous spread of COVID-19 across rural America is explored.
Rural Americans are especially at risk for a second wave of the coronavirus because they lack the medical facilities of more urban centers and have seen stay-at-home orders lifted more quickly during the initial round of COVID-19 infections.
#9 – Unprepared: Oregon
Like Maine, Oregon is, perhaps more than people would initially think, a largely rural state. Outside of the Portland area, Oregonians have less access to medical facilities and face relatively high rates of asthma.
Oregon Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 4.218 million | 17.6% | 11.6% | 29.9% | 1.6 | 303.4 | 8.2% |
“Reopening any part of our state comes with risk,” Oregon Governor Kate Brown explained in a recent press conference, adding:
“This virus is still very dangerous and it still poses a great threat. Until there is a vaccine, unfortunately, we will not be going back to life as we knew it. Not here in Oregon or frankly anywhere. I know this can be a really tough reality to face.”
#8 – Unprepared: West Virginia
Though West Virginia has a low share of uninsured residents, it has a much higher-than-average share of residents with asthma, those who are obese, and people over the age of 65.
West Virginia Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 1.792 million | 19.9% | 12.3% | 39.5% | 3.8 | 263.4 | 7.5% |
In the first round of COVID-19 infections, West Virginia was one of the last states to report coronavirus cases due to inadequate testing. As you can see in the video from NBC News below, the state now worries that hospitals will struggle as the pandemic continues and returns again in the fall.
Largely rural states like West Virginia face unique challenges when it comes to preparing for a public health crisis. They also rely more on federal resources to meet public health needs than more-densely populated states.
Read More: Albright, West Virginia Medicare Companies and Plans
#7 – Unprepared: Arkansas
Arkansans lack access to doctors and face high rates of obesity, which puts them more at risk when it comes to the second wave of the COVID-19 pandemic, or public health crises more generally.
Arkansas Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 3.018 million | 17% | 9.8% | 37.1% | 3.2 | 207.6 | 9.3% |
Some good news for the Natural State: More Arkansans have health insurance on average than most states on this list, and the state has a relatively high number of active physicians per capita.
#6 – Unprepared: Mississippi
Though Mississippians have more hospital beds per capita than almost any other state across the country, they also have some of the highest obesity and uninsured rates.
Mississippi Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 2.976 million | 15.9% | 9.7% | 39.5% | 4 | 191.3 | 14.5% |
Hospital beds do little good if you don’t have the insurance to put them to use. American Public Media’s In the Dark podcast is running a special series on COVID-19 in Mississippi, “Coronavirus in the Delta,” and it provides a wealth of insight into the special medical needs of the Hospitality State.
#5 – Unprepared: South Carolina
South Carolina has a fairly high share of its population over the age of 65, as well as a relatively high rate of obesity and a large number of uninsured residents.
South Carolina Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 5.149 million | 17.7% | 9.1% | 34.3% | 2.4 | 229.5 | 13.1% |
As South Carolinians have sheltered at home during the first wave of the coronavirus outbreak, there have been many surprises. As you can see in the video below, the Lossada family of Hilton Head had a surprise visitor in their backyard.
Luckily neither George the Gator nor any of the Lossadas was harmed by this cross-species encounter. Though rural coastal areas such as Hilton Head have been relatively spared during the first wave of the coronavirus, it is important for residents in such places to keep as vigilant in keeping the virus at bay as they do alligators and other unexpected guests.
You might not be susceptible to gator visits where you live, but your household might be one of the 67 percent of American households with a pet. COVID-19 has been found to affect many pets, especially dogs and cats, so it might be a good time to ask: Is pet insurance worth the cost?
#4 – Unprepared: Arizona
Heading to the American Southwest, we’re ranking Arizona as the fourth least-prepared state to face the second wave of COVID-19 infections.
Arizona Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 7.279 million | 17.5% | 10% | 29.5% | 1.9 | 242 | 12.1% |
Arizona is a large state with a vast majority of its population living in one area. The Phoenix-Mesa-Scottsdale metropolitan statistical area is home to 4.561 million of Arizona’s 7.279 million residents. With so many Arizonans not living in this metropolis, that means many folks have a harder time accessing medical facilities.
#3 – Unprepared: Alabama
With high rates of both obesity and asthma, Alabama lands at the third spot on our list of states least-prepared to face the second wave of the COVID-19 pandemic.
Alabama Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 4.903 million | 16.9% | 10.5% | 36.2% | 3.1 | 217.1 | 11% |
A good portion of Alabama’s tourism dollars come from the Gulf Shore beaches on the state’s southern shore. As you can see in the video below, social distancing is hard to police on these beaches.
Unfortunately, reopening such beaches and seeing a surge in visitors may help contribute to the spread of the coronavirus, especially as we face a second wave of the pandemic at the end of the summer and into the fall.
#2 – Unprepared: Oklahoma
Though it has a relatively young population, Oklahoma also has one of the highest uninsured rates in the United States. With 34.8 percent of the population battling obesity, the Sooner State also ranks high in one of the risk factors the CDC is most concerned about when it comes to quickly-spreading viruses like COVID-19.
Oklahoma Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 3.957 million | 15.7% | 10.3% | 34.8% | 2.8 | 206.7 | 16.5% |
Oklahoma is home to over 533,000 Native Americans. In the video from Johns Hopkins Bloomberg School of Public Health below, you can learn about the high risk that COVID-19 poses to Native American communities.
As you can see, Native American communities often lack access to both health care itself as well as vital health education. The Indian Health Service—the federal government’s agency for American Indians and Alaska Natives—exists to provide health care services to Native Americans in federal hospitals and is a valuable resource for a large share of Oklahoma’s population.
#1 – Least Prepared State: New Mexico
Topping our list of the states least-prepared for the second wave of COVID-19 is New Mexico, the Land of Enchantment. Like many states on this list, New Mexico’s medical infrastructure suffers from a large urban-rural divide.
New Mexico Statistics
| Population | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents |
|---|---|---|---|---|---|---|
| 2.097 million | 17.5% | 9.9% | 32.3% | 1.8 | 244.8 | 11% |
As you can see, New Mexico has a quickly aging population with below-average access to hospital beds or practicing doctors. This is especially true for New Mexicans living outside of the Albuquerque metropolitan area, which is home to nearly half of the state’s population.
As you can see in the video below from PBS News Hour, rural healthcare systems are already strained.
As we face another wave of the COVID-19 pandemic, public health officials worry rural healthcare systems could be strained to their breaking point.
Sadly, the coronavirus pandemic has us asking some tragic, but good questions such as where is my nearest emergency room, and how does life insurance work?
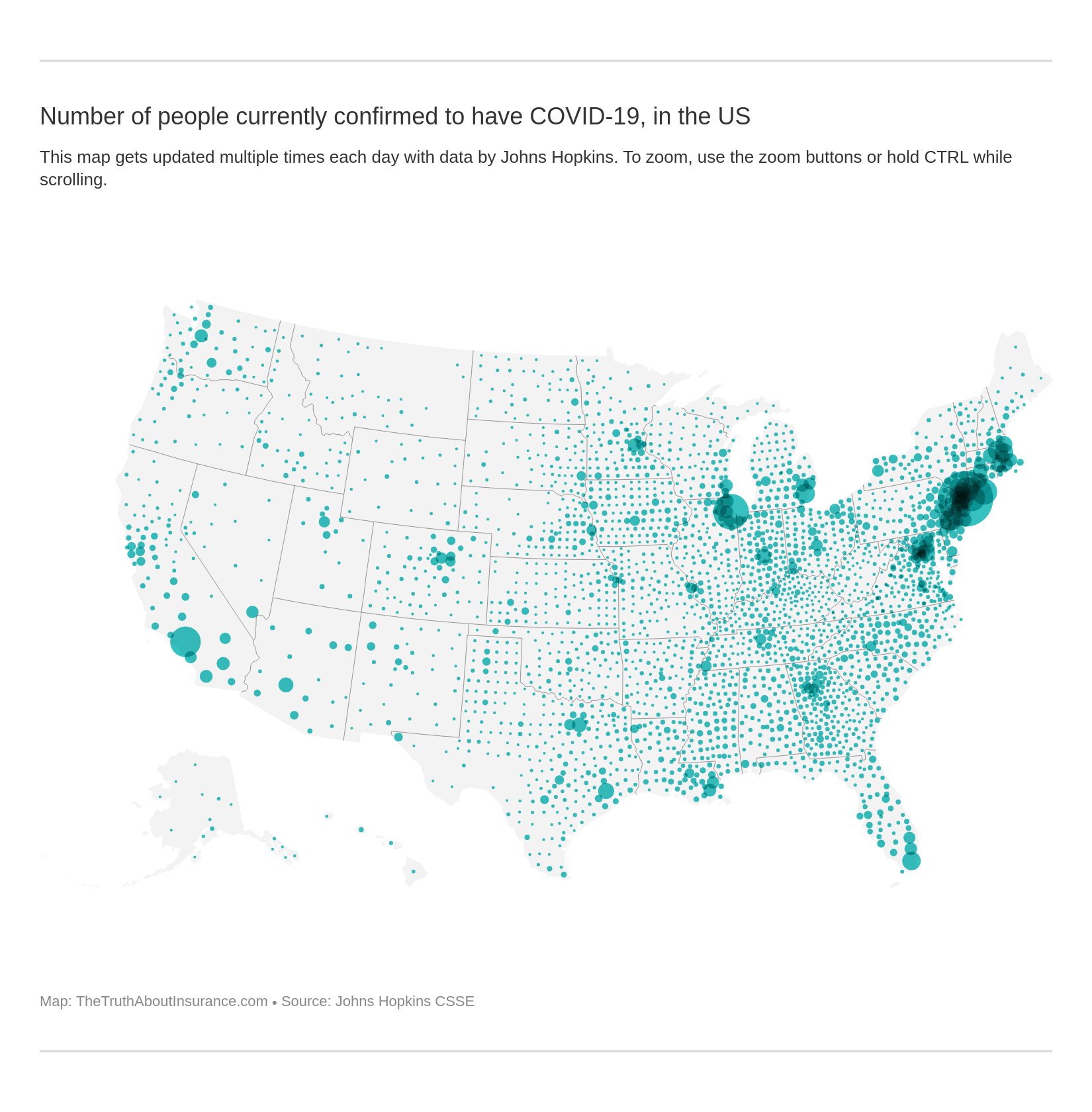
Confirmed Cases of COVID-19 Across America
The current coronavirus pandemic is still largely concentrated in densely-populated urban areas, as evidenced in the interactive map below. This map is updated daily with data from Johns Hopkins University.
COVID-19 second wave news shows that though COVID-19 is still largely concentrated in major cities, as the coronavirus continues to spread, the number of cases in rural areas is also growing.
States like Arizona, Arkansas, and Texas have seen recent rises in coronavirus infections, especially following the Memorial Day holiday weekend. Crowded parties—such as the one at Missouri’s Lake of the Ozarks featured in the NBC Nightly News video below—are potential hotspots that worry public health officials and epidemiologists across the United States.
As more businesses and activity centers begin to reopen across the country, COVID-19 second wave predictions are that we can expect cases to continue to rise in areas with less-strict containment measures in place. These lacking regulations put states more at risk for a second wave of COVID-19 infections if they aren’t following COVID-19 second wave CDC guidelines.
Compare Quotes From Top Companies and Save Secured with SHA-256 Encryption
Professionals Discuss Preparation for COVID-19’s Second Wave
In the video below, Dr. Marc Lipstich, Professor of Epidemiology at Harvard’s T.H. Chan School of Public Health, discusses strategies for mitigating a second wave of the coronavirus with Dr. Howard Bauchner, editor-in-chief of the Journal of the American Medical Association (JAMA).
We asked a variety of professionals—including public health advocates and lawyers—to weigh in on preparing for the coronavirus’s second wave. Read on to find out what they had to share.
Officials report that the second wave of the coronavirus could be just as bad as the first, if not worse. Do you agree with this assessment, and why?
“COVID-19 is so new that no one can be completely sure what a second wave will look like. However, my gut instinct tells me that any future waves won’t be as bad. Even if the virus is just as deadly and spreads just as quickly, people will have seen it coming.
Fewer people will panic shop and hopefully, more people will have basic supplies on hand. However, if people get too comfortable with the idea of a pandemic before a second wave hits, those waves could be worse since fewer people will follow social distancing guidelines.”
What tips do you have for our readers about individual preparedness for a second wave of the COVID-19 virus outbreak?
“People should use COVID-19 as a wake-up call about preparedness in general. Global pandemics might not occur frequently, but natural disasters like earthquakes, hurricanes, and flooding are regular occurrences.
There are also personal disasters like illness and unemployment that can be equally devastating. To make sure you are ready for pandemics as well as any other disaster situation, you’ve got to cover all of the essentials.
These essentials include: food, water, first aid, hygiene, heating, lighting, self-defense and safety, disaster cleanup, and evacuation. You’ll find that pandemic supplies like N95 face masks are useful to have during hurricane cleanup. Hand sanitizer is a must-have when in an evacuation shelter. And a two-week supply of emergency food is necessary for blizzards.”
Do you have any stories you can share about preparedness or lack thereof to this pandemic?
“I’m active in a lot of prepping groups. These are people who have been preparing for disasters for years. However, the pandemic was the first time most of them really had their preps put to the test. Most people found that, while they had enough food, they didn’t have enough of the foods they actually wanted to eat.
This time around, they are going to stockpile more ‘luxury’ items like coffee, creamer, chocolate, and alcohol.
The run on toilet paper also came as a big surprise. Because of the pandemic, I personally decided to stop using toilet paper for pee. Instead, I have a basket of clean cloth towels next to the toilet. I use these for wiping (I still use TP for poo) and then put them into a separate basket for laundering.
Another big issue which a lot of preppers experienced was not having enough extra supplies for friends and family. It was really hard to say ‘no’ to people asking for some hand sanitizer or a mask. If your loved ones aren’t on board with prepping, you might want to stockpile some extras for them just in case.”
Diane Vukovic, writer for PrimalSurvivor.net, is the author of Disaster Preparedness for Women.
Diane is a prepping expert who gives actionable advice about preparing for disasters.
“Some of the elements that make an area prepared or not prepared to face a pandemic would be to have the proper equipment to contain an outbreak. This equipment includes masks, hand sanitizers, gloves, and protective wear.
Additionally, we need adequate testing mechanisms and the ability to treat people should individuals become infected with the coronavirus. This mechanism might be containment or isolation of infected individuals.
I believe that a second wave is almost certain; however, I do not think it will be as bad. I think we are now more prepared to handle a second wave with protective gear and the general public has a better understanding of what a pandemic is and how to control its spread. When the first wave of the coronavirus came about, it blindsided almost everyone.
I think that governments and public agencies can work together with private entities such as hospitals or NGOs to combat a pandemic by sharing resources and information. The resources might be, but would not be limited to, protective gear and information about outbreaks as they develop.
Making the public aware of what spreads a pandemic is a major measure that my state, New York, is carrying out. More education is out there on how and what causes a pandemic to spread. However, there is a lack of consistency and much information out there which is contradictory. I am concerned that this will continue moving forward.
I suggest that to be prepared for the second wave of the COVID-19 outbreak to always err on the safe side. Wear a mask, maintain social distancing, and treat the moment as though we are in a full scale, out of control pandemic. Since the virus is invisible it is almost impossible to detect if the virus is being spread.
In the midst of the first wave, I was living in New York City with my wife and two small children, ages 5 and 9. As the city began to shut down and the virus began to rage, I knew that we had to leave the city. We were not prepared for what was about to happen, however, I knew that we needed to get out of the city.
The way we prepared was to empty our apartment out and leave the city within 12 hours. We got masks and protective gear and took a plane to the desert away from people in a more controlled environment. There was no way to prepare, but moving forward, I would continue to maintain social distancing, wash hands, and eat at home.
I do not trust the wild variations in news and would rather be on the safe side. So how I will prepare is to treat the situation as though the virus was at my doorstep every day until a vaccine becomes available.
I am a personal injury attorney and am in fact bringing claims on behalf of my clients for business interruption. We fight to bring justice to our clients especially in these difficult times.”
Evan Oshan is an award-winning attorney and the founder of Oshan & Associates P.C.
Evan, recognized as a Top 100 Lawyer, secures high profile, multi-million-dollar cases.
“The prediction by health officials regarding the second wave of COVID-19 is totally correct. I have no concern about it because I’m practically watching the outcome, as earlier portrayed in the reports.
I reside in the metropolitan city of Pakistan, namely Karachi. We have just entered the second phase of this pandemic, and the cases have jumped to 89,244 from 30,000 with a recorded death toll of 1,838 as of the 5th of June.
According to the health ministry of Punjab (Pakistan’s largest province in terms of population), the estimated actual figures could be 300,000 solely in the region.
After staying home for two consecutive months (March and April), my company asked me to resume work at home in the wake of a declining rate as the figure was just around 15,000 at that time. I resumed work at the office, but unfortunately, in the mid of May, the cases increased so dramatically that my company has once again asked me to work from home.
Now the situation is that there is no market, area, office, or street where this virus doesn’t exist. Even in my social circle, many people have found to be affected by this virus, or have relatives diagnosed with coronavirus. Not only this, but also the private hospitals have even refused to treat any COVID case to prevent their patients and medical staff from catching it.
To get over this chaotic situation, the Government of Pakistan has introduced a force of volunteers called ‘Tiger Force.’ The force is responsible for distributing groceries, creating awareness among the masses, and encouraging the culture of social distancing. Tigers are trained to work like military officials to deal with the worst situations.
A big Tiger Force responsibility is to secure the military personnel who are not affected by COVID-19 yet. The government of Pakistan is wisely handling the situation to keep the armed forces out of this pandemic.
The only way to prevent yourself from this potentially deadly virus is to practice three things religiously. Those three things are:
- social distancing
- wearing masks and gloves
- washing your hands
This must be done every time you get back home. Additionally, you should compulsively ask your employer to allow you to work from home, if possible.”
Ammar Shahid is a digital marketing executive with SuperHeroCorp.
Shahid runs digital marketing campaigns through content and influencer marketing.
“As a technology vendor, Relatient provides solutions for health care staff to text patients, allowing them to wait in their car until ready for an appointment, fill out paperwork, and make payments on their phones.
Telehealth is also playing a huge role in helping patients get care at home. Many businesses are still asking that employees work from home if possible, Relatient included. Others have adopted safety policies that include regular cleaning and mask-wearing.
Tips for preparedness:
Encourage more telehealth and contactless interactions like what providers are now beginning to offer. Have a plan with your doctor, and don’t forget your normal care. Ask what they’re doing to make it safer. Can you do telehealth?
At Relatient we quickly changed strategy from generating new sales to helping customers utilize the patient communication tools we offer them to prepare their patients for changes. In the first month customers sent out over 7 million messages to patients just about COVID-19.
Some customers had telehealth solutions, others didn’t but moved extraordinarily fast to implement. We worked with customers to incorporate telehealth into their patient outreach.”

Relatient improves the quality of health care with better provider-to-patient communication.
Compare Quotes From Top Companies and Save
Secured with SHA-256 Encryption
Frequently Asked Questions: COVID-19
There are a lot of questions surrounding the coronavirus and how states are preparing, or not preparing, to face the second major round of infections. Let’s take a look at some of these additional questions.
#1 – When will the second wave of COVID-19 hit?
Given that most states are reopening in major ways, a second wave of coronavirus infections may be closer than you think. San Francisco’s ABC 7 recently reported that:
“Health officials have long been warning of a second wave of coronavirus cases to come sometime in the fall, but a global spike may come even sooner. While new infections may be on the decline in Europe, Asia and North America, the World Health Organization’s Dr. Mike Ryan warned that trend may change with loosened restrictions.”
#2 – How much longer will the coronavirus outbreak last?
Most reputable health organizations agree: COVID-19 may now be a permanent part of our lives. The virus is not likely to disappear completely, and our daily lives will likely not return to some sense of normalcy until a vaccine is developed.
#3 – Is there a vaccine for the coronavirus?
Sadly, not yet. The U.S. Food and Drug Administration’s (FDA’s) Center for Biologics Evaluation and Research (CBER) is responsible for regulating vaccines in the United States, and they are working diligently with a variety of agencies and organizations to bring a vaccine to market.
#4 – How long does it take for symptoms of the coronavirus disease to appear?
According to the World Health Organization (WHO), “on average it takes 5–6 days from when someone is infected with the virus for symptoms to show. However, it can take up to 14 days.”
#5 – How can I track the coronavirus outbreak?
Good question. Johns Hopkins University is currently tracking confirmed cases of COVID-19 around the world. They offer an interactive map that is updated daily. You can also see their data in our interactive map above, which is also updated daily.
#6 – Have traffic and roadway usage been affected by COVID-19?
In short: Absolutely. In many places, roadway usage has fallen 50 percent or more as people work remotely and live with stay-at-home orders or advisories. You can track the effect of the coronavirus on traffic and roadway usage through the in-depth and interactive “Live Coverage of COVID-19 Transportation Trends” from INRIX, one of the leading traffic monitoring agencies.
#7 – Is COVID-19 going away?
Although the coronavirus is still spreading throughout the world, with different countries undergoing different measures to prevent the spread, medical experts state that Americans and residents of other states around the world will soon have access to a vaccine or better treatment, which means we won’t spend our entire lives in global pandemic due to the coronavirus.
#8 – Is there a vaccine for coronavirus?
As of now, there is no vaccine that has been fully tested and available on the market. Some countries, such as Russia and China, have approved vaccines for preliminary use in their own countries. However, these are still listed in the World Health Organization’s database as “under testing.”
#9 – Should I be tested for COVID-19?
As the CDC would say, “Maybe.” Not everyone needs to be tested for COVID-19, including those perhaps with very mild symptoms like a headache, a sore throat, or a little fatigue. There are more serious symptoms like struggling to breathe that health experts will often say require medical input or recommendations. In general, these situations depend on you and your doctor as well as the established medical practices in your community or in respect to your personal health situations.
#10 – What are the symptoms of COVID-19 and how long does it take for them to appear?
The symptoms of COVID-19 include fatigue, headache, sore throat, clogged nose, slight fever, loss of sense of taste and smell, body aches or chills, and difficulty breathing. It generally takes between two and 14 days for the first symptoms to appear. However, some people can catch COVID-19 and not present any symptoms at all.
#11 – Can you contract the coronavirus disease from a package in the mail?
While there is some evidence that the coronavirus disease can remain on surfaces for a short amount of time, the CDC states that it is unlikely that you will contract the coronavirus disease from handling packages through the mail, whether those are domestically- or internationally-shipped packages.
#12 – Is a headache sign of the coronavirus disease?
Headache is a common symptom of COVID-19 along with other common symptoms like fatigue and sore throat. In general, most health organizations note that, while these symptoms can be unsettling, they also occur in other, related but not as dangerous viruses, like the flu or the common cold. If you have any concerns, reach out to your doctor or your city’s local line that handles possible coronavirus cases.
#13 – Can antibiotics treat the coronavirus disease?
Because antibiotics treat bacterial infections and the novel coronavirus is a virus, antibiotics can not be used to treat the coronavirus. As of now, there is no FDA approved treatment for the coronavirus, though doctors and hospitals around the country have been using various treatments since the pandemic began to treat patients with the coronavirus.
Complete Rankings: Pandemic Preparedness State by State
We know it’s helpful to see the states ranked by on coronavirus preparedness all in one easy-to-read spot.
In the table below, we’re offering our data on each state’s preparedness to face a second wave of the COVID-19 pandemic and their ranking of preparedness, from most- to least-prepared.
COVID-19 Second Wave: State Preparedness
| State | Population Ages 65+ | Population with Asthma | Population Facing Obesity | Hospital Beds Per 1,000 People | Active Physicians Per 100,000 People | Uninsured Residents | Rank |
|---|---|---|---|---|---|---|---|
| Minnesota | 15.9% | 8.3% | 30.1% | 2.5 | 302.7 | 5.1% | 50 |
| New Jersey | 16.1% | 8.4% | 25.7% | 2.4 | 306.5 | 9.0% | 49 |
| Massachusetts | 16.5% | 10.2% | 25.7% | 2.3 | 449.5 | 3.3% | 48 |
| New York | 16.4% | 10.1% | 27.6% | 2.7 | 375.1 | 6.6% | 47 |
| California | 14.3% | 8.5% | 25.8% | 1.8 | 279.6 | 8.2% | 46 |
| Colorado | 14.2% | 9.1% | 23.0% | 1.9 | 285.7 | 8.7% | 45 |
| Illinois | 15.6% | 8.7% | 31.8% | 2.5 | 284.4 | 7.9% | 44 |
| North Dakota | 15.3% | 8.2% | 35.1% | 4.3 | 237.6 | 8.6% | 43 |
| Maryland | 15.4% | 9.3% | 30.9% | 1.9 | 386.0 | 7.0% | 42 |
| South Dakota | 16.6% | 2.9% | 30.1% | 4.8 | 240.4 | 10.8% | 41 |
| Hawaii | 18.4% | 9.3% | 24.9% | 1.9 | 314.1 | 4.6% | 40 |
| Virginia | 15.4% | 8.5% | 30.4% | 2.1 | 263.2 | 10.2% | 39 |
| Nebraska | 15.7% | 8.9% | 34.1% | 3.6 | 239.2 | 9.6% | 38 |
| Louisiana | 15.4% | 8.9% | 36.8% | 3.3 | 260.3 | 9.6% | 37 |
| Washington | 15.4% | 9.6% | 28.7% | 1.7 | 278.8 | 7.1% | 36 |
| Rhode Island | 17.2% | 11.9% | 27.7% | 2.1 | 370.0 | 5.4% | 35 |
| Pennsylvania | 18.2% | 10.0% | 30.9% | 2.9 | 320.5 | 6.6% | 34 |
| Connecticut | 17.2% | 10.3% | 27.4% | 2.0 | 352.1 | 6.3% | 33 |
| Alaska | 11.8% | 9.2% | 29.5% | 2.2 | 276.9 | 14.8% | 32 |
| Ohio | 17.1% | 9.4% | 34.0% | 2.8 | 292.7 | 7.1% | 31 |
| Iowa | 17.1% | 7.9% | 35.3% | 3.0 | 218.2 | 5.5% | 30 |
| Wisconsin | 17.0% | 9.0% | 32.0% | 2.1 | 264.9 | 6.4% | 29 |
| Wyoming | 16.5% | 8.7% | 29.0% | 3.5 | 207.9 | 14.2% | 28 |
| Vermont | 19.4% | 12.0% | 27.5% | 2.1 | 367.1 | 5.5% | 27 |
| Utah | 11.1% | 9.3% | 27.8% | 1.8 | 216.2 | 10.0% | 26 |
| Montana | 18.7% | 10.0% | 26.9% | 3.3 | 247.1 | 10.4% | 25 |
| Michigan | 17.2% | 11.2% | 33.0% | 2.5 | 287.0 | 6.1% | 24 |
| Nevada | 15.7% | 8.0% | 29.5% | 2.1 | 213.5 | 13.1% | 23 |
| Georgia | 13.9% | 8.9% | 32.5% | 2.4 | 228.7 | 15.5% | 22 |
| Texas | 12.6% | 7.4% | 34.8% | 2.3 | 224.8 | 19.4% | 21 |
| Missouri | 16.9% | 9.4% | 35.0% | 3.1 | 273.1 | 10.9% | 20 |
| New Hampshire | 18.1% | 11.8% | 29.6% | 2.1 | 315.1 | 7.0% | 19 |
| Kansas | 15.9% | 9.8% | 34.4% | 3.3 | 227.6 | 10.1% | 18 |
| Indiana | 15.8% | 10.0% | 34.1% | 2.7 | 230.8 | 9.6% | 17 |
| Idaho | 15.9% | 8.6% | 28.4% | 1.9 | 192.6 | 11.8% | 16 |
| Kentucky | 16.4% | 11.5% | 36.6% | 3.2 | 230.9 | 6.4% | 15 |
| Tennessee | 16.4% | 9.8% | 34.4% | 2.9 | 253.1 | 11.3% | 14 |
| Delaware | 18.7% | 10.1% | 33.5% | 2.2 | 284.6 | 6.1% | 13 |
| Florida | 20.5% | 8.7% | 30.7% | 2.6 | 265.2 | 16.0% | 12 |
| North Carolina | 16.3% | 9.4% | 33.0% | 2.1 | 255.0 | 12.6% | 11 |
| Maine | 20.6% | 12.3% | 30.4% | 2.5 | 330.2 | 10.2% | 10 |
| Oregon | 17.6% | 11.6% | 29.9% | 1.6 | 303.4 | 8.2% | 9 |
| West Virginia | 19.9% | 12.3% | 39.5% | 3.8 | 263.4 | 7.5% | 8 |
| Arkansas | 17.0% | 9.8% | 37.1% | 3.2 | 207.6 | 9.3% | 7 |
| Mississippi | 15.9% | 9.7% | 39.5% | 4.0 | 191.3 | 14.5% | 6 |
| South Carolina | 17.7% | 9.1% | 34.3% | 2.4 | 229.5 | 13.1% | 5 |
| Arizona | 17.5% | 10.0% | 29.5% | 1.9 | 242.0 | 12.1% | 4 |
| Alabama | 16.9% | 10.5% | 36.2% | 3.1 | 217.1 | 11.0% | 3 |
| Oklahoma | 15.7% | 10.3% | 34.8% | 2.8 | 206.7 | 16.5% | 2 |
| New Mexico | 17.5% | 9.9% | 32.3% | 1.8 | 244.8 | 11.0% | 1 |
Methodology: State Ranking by Pandemic Readiness
To rank the 10 states most at-risk for a second COVID-19 wave, we took into account several points of data:
- States with the highest percentage of their population over the age of 65
- States with the highest rates of asthma
- States with the highest rates of severe obesity
- States with the fewest number of hospital beds per capita
- States with the fewest active physicians per capita
- States with the highest percentage of uninsured individuals
We tabulated our rankings of the states most and least at risk for a second wave of coronavirus on six areas of data with research from reputable leaders in public health and demographic health research: the Centers for Disease Control and Prevention (CDC), the U.S. Census Bureau, the American Medical Association, the Kaiser Family Foundation, and Becker’s Hospital Review.
The thorough research process for our comprehensive studies, such as this one on state preparedness for the coronavirus pandemic, includes an analysis of over 8,000 data points for all 50 U.S. states and the District of Columbia from a variety of government, nonprofit, academic, and industry sources.
Ready to compare rates before the COVID-19 second wave hits your area? Put your information into our FREE online quote generator to compare the best rates for you and your area.
Compare Quotes From Top Companies and Save
Secured with SHA-256 Encryption
Jeff Root
Licensed Insurance Agent
Jeff is a well-known speaker and expert in life insurance and financial planning. He has spoken at top insurance conferences around the U.S., including the InsuranceNewsNet Super Conference, the 8% Nation Insurance Wealth Conference, and the Digital Life Insurance Agent Mastermind. He has been featured and quoted in Nerdwallet, Bloomberg, Forbes, U.S. News & Money, USA Today, and other leading...
Licensed Insurance Agent
Editorial Guidelines: We are a free online resource for anyone interested in learning more about life insurance. Our goal is to be an objective, third-party resource for everything life insurance related. We update our site regularly, and all content is reviewed by life insurance experts.